-
Services
Featured Services
-
Locations
Location Type
Hospitals and Multispecialty Locations
-
Patients & Visitors
Greenwich Hospital offers two, minimally invasive (i.e. laparoscopic) Bariatric surgical procedures.
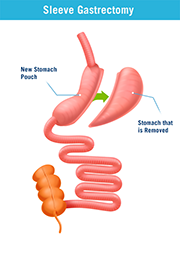
Laparoscopic sleeve gastrectomy is particularly well-suited for those at the highest risk for surgery, either because of their medical history or their weight. Under certain conditions, it is also offered as a first-step, lower-risk bridge to other bariatric operations. The procedure involves removing 80 percent of the stomach, leaving only a tube or "sleeve" of stomach behind. This restricts the amount of food that a patient can eat, and often leads to significant weight loss, in addition to also changing hormone production related to hunger.
Enlarge image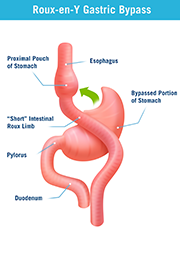
Roux-en-Y gastric bypass — one of the most common Bariatric surgeries — is a minimally invasive procedure that creates a smaller, golf ball-sized stomach out of the existing one. Having less space in the stomach means smaller amounts of food will make patients feel full, so they consume less. Also, by bypassing the larger portion of the stomach and rerouting the path to the intestine, food comes in contact with digestive juices for a shorter period of time, so less calories are absorbed. In addition, alteration of the stomach also causes changes in the hormones which help regulate appetite and hunger.
Enlarge imageOver time, some weight-loss surgery procedures may need to be revised due to complications or failure to lose weight. Greenwich Hospital performs revisional surgeries which range from correction of issues leading to complications, to conversion from one weight-loss procedure to another which better suits the current medical conditions of the patient.
Whenever bariatric surgery is required as part of a comprehensive weight-loss strategy, the patient's surgeon will help decide which procedure is best. The final choice is based on a number of factors and eligibility requirements, including medical history, age, body mass index (BMI), and previous weight-loss treatment results. These same factors will also affect how much weight a patient can expect to lose after surgery.
Weight loss resulting from any of these procedures can significantly improve conditions associated with severe obesity, such as sleep apnea, diabetes, high cholesterol, gastroesophageal reflux disease (GERD) and high blood pressure. In fact, studies show that the risk of death from these conditions returns to normal after successful weight-loss surgery and obesity treatment.
The majority of weight-loss surgeries are performed laparoscopically, with several very small incisions using high definition video and special equipment and instruments. The benefits of laparoscopic surgeries are less discomfort, shorter hospital stay, earlier return to work and reduced scarring.
Statistically, the risk of death during these procedures is less than 1 percent. Your doctors will have assessed you for risks and prepared accordingly. All abdominal operations carry the risks of bleeding, infection in the incision, thrombophlebitis of legs (blood clots), lung problems (pneumonia, pulmonary embolisms), strokes or heart attacks, anesthetic complications and blockage or obstruction of the intestine. These risks are greater in patients with severe obesity.

Find out more about improving your health through weight-loss surgery by viewing our recorded informational webinar.

See how our experts are with you throughout your weight-loss journey.